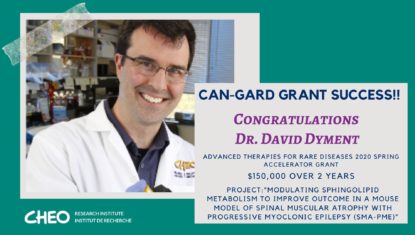
Dr. David Dyment is a clinical investigator at the CHEO Research Institute and Associate Professor at the University of Ottawa. He completed his graduate training in the genetics of complex disease at the University of Oxford and later medical training at the University of Calgary. His clinical interest is neurogenetics with a focus on epilepsy and he works as a clinician in the Neurogenetics program at CHEO.
His current research interests include the identification of genes for human malformation syndromes and also novel genes associated with forms of epilepsy. In addition, he has an active interest in model systems for Dravet syndrome and Spinal Muscular Atrophy and Progressive Myoclonic Epilepsy. He is the recipient of a CIHR Clinical Investigator award and has a University of Ottawa Tier 2 Research Chair in Epilepsy Genetics.
Related News
Research Projects
-
Evaluation of the diagnostic accuracy of exome sequencing and its impact on diagnostic thinking for patients with rare disease in a publicly funded health care system: A prospective cohort study
26/02/2024
The introduction of genomic technologies, such as exome sequencing (ES), has created an opportunity to shorten the uncertain and emotionally taxing “diagnostic odyssey” experienced by families with suspected rare genetic diseases (RGDs).1, 2, 3 A meta-analysis has demonstrated a diagnostic yield of 36% for both clinical and research-based ES in the context of a broad range of RGD indications.4 However, studies have typically been retrospective analyses on convenience samples of patients or large cohorts with unspecified phenotypes reported by diagnostic laboratories. Despite few randomized-controlled trials, systematic reviews, and health technology assessments, health care systems in various jurisdictions have moved to implement ES as a clinical test.5 How jurisdictions optimize this test’s implementation will depend on their health care system and context. However, sharing empirical evidence of the utility of this test and policy processes that support its use can guide health care systems in these implementation efforts.6
-
First reports of primary ciliary dyskinesia caused by a shared DNAH11 allele in Canadian Inuit
23/04/2023
The discovery of this homozygous DNAH11 variant in widely disparate parts of the Nunangat (Inuit homelands) suggests this is a founder mutation that may be widespread in Inuit. Thus, PCD may be an important cause of chronic lung, sinus, and middle ear disease in this population. Inuit with chronic lung disease, including bronchiectasis or laterality defects, should undergo genetic testing for PCD. Consideration of including PCD genetic analysis in routine newborn screening should be considered in Inuit regions.
-
Bridging clinical care and research in Ontario, Canada: Maximizing diagnoses from reanalysis of clinical exome sequencing data
01/03/2023
-
Outcome of over 1500 matches through the Matchmaker Exchange for rare disease gene discovery: The 2-year experience of Care4Rare Canada
01/01/2022
Matchmaking through the MME is an effective way to investigate novel candidate genes; however, it is a labor-intensive process. Engagement from the community to contribute phenotypic, genotypic, and inheritance data will ensure that matchmaking continues to be a useful approach in the future.
-
PLPHP deficiency: clinical, genetic, biochemical, and mechanistic insights
01/03/2019
The vitamin B6-responsive disorders (B6RDs) are a clinically and genetically heterogeneous group of rare, autosomal recessive conditions (Clayton, 2006) with the hallmark feature of seizures uniquely responsive to treatment by the B6 vitamers pyridoxine and/or pyridoxal-5′-phosphate (PLP) (Baumgartner-Sigl et al., 2007; Basura et al., 2009). PLP is a cofactor for over 160 distinct catalytic functions (Percudani and Peracchi, 2009), including enzymes involved in glucose, lipid and amino acid metabolism (John, 1995; Percudani and Peracchi, 2003; Eliot and Kirsch, 2004), and for the synthesis of neurotransmitters, making it an essential vitamer for normal brain function (Surtees et al., 2006).