22/09/2020
Ottawa, Ontario — Tuesday September 22, 2020
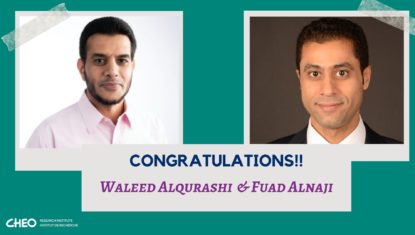
Waleed Alqurashi and Fuad Alnaji are co-applicants and the CHEO site-lead investigators for the study “Pragmatic Pediatric Trial of Balanced Versus Normal Saline Fluid in Sepsis (PRoMPT BOLUS)” which is lead out of the University of Calgary. The study received a $1.5 million grant from CIHR over 5 years. The PRoMPT BOLUS study will be the largest trial of pediatric-specific, ED-initiated sepsis management to address the important clinical question of efficacy and safety of crystalloid fluids.
Sepsis is a medical emergency caused by severe infection. Septic shock is the most severe form. More than 25 million children worldwide are diagnosed with sepsis/septic shock every year. Sepsis is the most expensive hospital condition in North America and for critically ill children is the most common cause of hospital death. The World Health Organization has called for optimized treatments in sepsis. Crystalloid fluid resuscitation is the cornerstone of initial treatment of sepsis. However, there is currently no research that clearly shows which is the most effective and safest type of crystalloid fluid in children. Two types of crystalloids are used for resuscitation in sepsis: balanced fluids (BF) and 0.9% “normal” saline (NS). In the absence of high quality, pediatric-specific data, NS resuscitation remains the overwhelming preference among pediatric emergency clinicians.
The objective of this large, pragmatic, randomized study is to test the comparative effectiveness of the two most common types of crystalloid (BF vs NS) to improve clinical outcomes in children treated for septic shock. Thirteen pediatric emergency departments in the Pediatric Emergency Research Canada (PERC) network will collaborate with sites in the United States, Australia, and New Zealand to enroll 8,800 children with suspected septic shock. Children will be randomized to receive fluid resuscitation and maintenance fluids with either NS or BF for 24-48 hours, with all other aspects of care (other than fluid type) at the discretion of the managing health care team. Our primary outcome is major adverse kidney events within 30 days from randomization (MAKE30), a patient-centered endpoint that includes persistent kidney dysfunction, initiation of dialysis, or death. An economic analysis will be completed.
